Anorectal Diseases
Content is being updated......

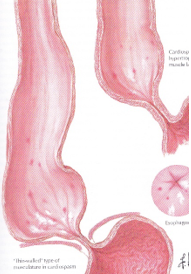
Esophageal diverticula; They are mucosal vesicles that have grown out of the esophageal lumen. Esophageal diverticula are classified according to their location, wall thickness and formation mechanism. According to their location, they are divided into 3 groups as pharyngoesophageal (ZENKER), parabronchial (gastric esophageal) and epinephric (supradiaphragmatic). Esophageal diverticula are the anatomical results of motor dysfunctions.
In the presence of symptoms, surgical intervention is required. The most important factor determining morbidity and mortality is aspiration.
It is usually between the ages of 30-50 and is the most common esophageal diverticulum. Cervical dysphagia and effortless regurgitation containing undigested food residues are the most common symptoms. Chronic cough, aspiration and recurrent lung infections are common complaints.

Diagnosis is made by barium esophagogram. Endoscopy has a risk of diverticular perforation. Surgical treatment is also the most appropriate treatment for pharyngoesophageal diverticulum. The diverticulum remaining after myotomy is sutured to the prevertebral fascia (diverticulopexy).
If the diverticulum is too wide and its wall is too thin, diverticulectomy is necessary. As a result, cricopharyngeal myitomy is an effective surgical treatment method that can be applied to any patient with Zenker disease, with extremely low morbidity.
These types of diverticula are typically associated with mediastinal granulomatous diseases (tuberculosis, histoplasmosis). These diverticula are usually asymptomatic and detected incidentally. Surgical treatment depends on the severity of the symptoms. These types of lesions are seen on the anterior wall of the esophagus and show adhesion to the surrounding tissues. Due to these dense adhesions, repairs are supported with pleural patches. It is recommended.
They are traction and pseudo-diverticula in the last 10 cm of the thoracic esophagus, which occur as a result of motor dysfunctions of the esophagus or mechanical distal obstruction. The symptoms are usually symptoms of the underlying esophageal disorder. Patients with severe, progressive dysphagia, chest pain and large diverticular pouch are candidates for surgery. Robotic, laparoscopic or thoracoscopic esophageal myotomy, diverticulectomy and funduplication procedures can be performed with similar success rates as open surgery.
Although it is a rare disease (incidence 1/100,000), it is the most common primary esophageal motility disorder and is common between the ages of 35-45.
Although the etiology of achalasia is unknown, motor dysfunction occurs in this disease due to destruction of the Auerbach's plexus.
Although the absence of peristalsis in the esophageal body is a major abnormality, current data suggest that achalasia is the primary disorder of the lower esophageal sphincter. The determining pathology is the insufficiency of the ganglia in the Auerbach's plexus.
Achalasia is divided into 3 clinical stages according to symptomatology and esophageal diameter; stage I
(esophagus <4 cm), stage II (esophagus 4-7 cm) and stage III (esophagus > 7 cm). Progressive dysphagia is present in almost all patients. Regurgitation (> 70%), odynophagia (retrosternal pain after swallowing) occur in 30% of patients. It is also present in the United States and consists of bronchitis and pneumonia (10%) that develop due to aspiration.
Achalasia is considered a premalignant lesion because it usually develops into squamous type esophageal cancer, which develops after an average of 15-25 years.
In barium esophagogram, there is a bird's beak appearance in the distal esophagus and enlargement in the proximal (Bird's Beak view).
Esophageal manometry is the most useful method in diagnosis. Characteristic manometric findings; It is the absence of peristalsis, the mirror image of contractions, and the absence of relaxation of the lower esophageal sphincter during swallowing. Endoscopy should be used to differentiate benign and malignant strictures.
The aim of medical treatment is to reduce the tone of the lower esophageal sphincter. For this purpose, nitrates, calcium channel blockers and, more recently, endoscopic injection of botulinum toxin into the lower esophageal sphincter region are used.
The other two treatment methods are pneumatic or hydrostatic forced dilation and esophagomyotomy. Extremely successful results have been achieved in 95% of patients with Heller esophagomyotomy. The successful result rate obtained with forced pneumatic dilatation is 65%. The potential complication of both methods is gastroesophageal reflux.
Surgical esophagomyotomy is used in four patient groups:
Partial fundoplication along with laparoscopic esophagomyotomy is used as the first choice.
Such patients have clinical and manometric features of achalasia and diffuse esophageal spasm. There is spastic pain and severe dysphagia caused by irregular peristalsis that occurs to overcome the lower esophageal sphincter that does not relax. The treatment is the same as for classical achalasia, but the esophagomyotomy must be kept longer.
It is the hypermotility of the esophagus, manifested by severe substernal pain and/or dysphagia. Its significant differences from classical achalasia are; DS is primarily a disease of the esophageal body. Dysphagia is milder, chest pain is more pronounced, and the general condition of the patient is less deteriorated. The primary symptom is severe chest pain that occurs at night or spontaneously. The character of chest pain is similar to angina pectoris seen in coronary artery disease.
Gallstones, ulcer disease, gastritis, pancreatitis may trigger EOS. Dysphagia, regurgitation and weight loss constitute other symptoms. Esophageal manometry is the most valuable method in diagnosis. Simultaneous, multiphasic, repetitive, prolonged and high amplitude contractions are usually observed.
Antispasmodics, calcium channel blockers and nitrates can be used in medical treatment. Pneumatic dilatation is not recommended because it may cause tears. Although esophagomyotomy is recommended, results have not been as successful as in achalasia.
It is a hypermotility disorder of the esophagus, characterized by manometrically prolonged, high-amplitude peristaltic waves and chest pain that mimics cardiac symptoms. Diagnosis and treatment methods are similar to achalasia and DS, but esophagomyotomy has not been shown to be beneficial.
This disorder is characterized by high LES pressure and normal relaxation and pushing movements of the esophageal body.
Some patients complain of chest pain and dysphagia, show abnormal waves and contractions in esophageal manometry, but do not meet the criteria for primary esophageal motor disorder.
They are motility disorders that develop as a result of the response of the esophagus to systemic diseases such as scleroderma, multiple sclerosis, diabetic neuropathy and inflammatory injuries.
Scleroderma: It is a systemic disease that progresses with loss of esophageal peristalsis in 80% of patients. It is twice as common in women and occurs between the ages of 30-40. Events begin with inflammation in small vessels. Smooth muscle atrophy is evident in the gastrointestinal system. Fibrosis of esophageal smooth muscles causes gastroesophageal reflux. Initially, patients begin to complain about the slow emptying of the esophagus, the need for water to move food through, and a burning sensation and reflux. Severe reflux esophagitis occurs with the delay in clearing the esophagus from food residues. Diagnosis of scleroderma is made by manometric and acid reflux tests. Shortening of the esophagus due to reflux esophagitis is often observed. After surgery, the contact of the esophagus with acid is interrupted. Good results can be achieved with transhiatal esophagectomy and cervical esophagogastrostomy in selected patients with advanced esophageal stricture, reflux esophagitis, dilatation and who do not respond to medical treatment.
The majority of esophageal perforations are iatrogenic injuries that occur during diagnosis and treatment procedures and constitute 60% of all esophageal perforations. Esophageal perforations can be grouped under 2 headings as intraluminal or extraluminal causes. The general mortality rate in esophageal ruptures is around 20%. 70% of patients with esophageal perforations are Pain is present in 90% of cases and is the most common symptom. Additionally, dysphagia, fever and progressive leukocytosis, tachycardia, respiratory distress and, if left untreated, shock may be detected.
Neck stiffness and subcutaneous cervical emphysema can be seen in cervical perforations, and mediastinal emphysema, chest pain, dyspnea and pleural effusion can be seen in thoracic perforations. Intra-abdominal perforations are accompanied by signs of peritonitis. In cases where a definitive diagnosis cannot be made, CT can be used. Endoscopy cannot directly see small perforations and may cause errors in diagnosis. .
The first step of successful treatment is early diagnosis. If the diagnosis can be made within the first 24 hours, 80-90% successful results can be achieved with primary repair. Treatment of cervical or upper thoracic esophageal perforations is drainage alone or primary repair with drainage. Thoracic perforations are repaired primarily and the perforation area is intact. It is supported by patching with tissues and mediastinal drainage is provided.
Plummer-Vinson or Patterson-Kelly Syndrome (sideropenic dysphagia)
Atrophic oral mucosa, spoon-shaped fingers, easily broken nails and chronic anemia are seen with dysphagia. The cause of dysphagia is the cervical esophageal web (membrane, curtain). Treatment is the correction of iron deficiency and dilatation of the web.
Schatzki Ring (Distal Esophageal Web)
Schatzki ring is a thin, circumferential ring seen at the squamocolumnar junction in the lower esophagus and is usually associated with a sliding hiatal hernia. Its prevalence in the general population is between 0.2-14%. It is a pleat formed by mucosal folding in the shortened esophagus, is congenital, and is associated with inflammatory stricture due to chronic reflux. It is claimed that the treatment results in intermittent bouginage and medical antireflux treatment. In patients with resistant dysphagia and gastroesophageal reflux symptoms resistant to drug treatment, the antireflux procedure together with intraoperative dilatation provides a significant improvement.
Mallory-Weiss Syndrome (Emetogenic Mucosal Laseration)
Increased intra-abdominal pressure due to extremely forceful vomiting when the glottis is closed is reflected in the esophagus and may cause mucosal (Mallory-Weiss syndrome) or transmural tears (Boerhaave Syndrome). This syndrome is also responsible for 15% of acute upper gastrointestinal tract bleeding. In the diagnosis, endoscopy diagnoses a herniated stomach along with a tear in the mucosa. Surgical intervention is required to stop bleeding in only a small number of patients.
Infectious Esophagitis
It is a clinical condition encountered in patients with general health problems, suppressed immune systems, or those who have used antibiotics for a long time. The most common cause of infectious esophagitis is Candida albicans.
Caustic Injuries
Accidental caustic injuries usually occur in children. Most of the injuries seen in adults are intentional or suicidal. There are three endoscopic periods in corrosive lesions. The first period is the acute necrosis period and continues for 1-4 days. The second period is the ulceration and granulation period, continues for 10-12 days, and the third period is the cicatrization period. Pain in the mouth or substernal region, excessive salivation, pain when swallowing, dysphagia, sometimes bleeding and vomiting are common findings.
If the cause of the incident is strong acids, serious systemic and respiratory problems and complications may occur. Treatment is directed to the early and late results of caustic injury. Neutralizing agents can be used within the first hour, but vomiting should not be induced. Hypovolemia is corrected and broad-spectrum antibiotics are given. In cases of extensive necrosis, esophageal resection, cervical Esophagostomy, nutritional jejunostomy, and reconstruction at 90 days or later are the best treatment. The most important problem in the late period is the risk of cancer development, which is 1000 times higher than in the normal population.
They are rare. The most common are leiomyomas, followed by polyps. Rarely encountered benign tumors are hemangiomas and granular cell myoblastoma.
They show symptoms depending on the location of the tumor. Intraluminal tumors such as polyps cause dysphagia, vomiting and aspiration due to obstruction. Intraluminal tumors such as leiomyoma are usually asymptomatic, but when they reach sufficient volumes, they cause dysphagia and chest pain. They can be diagnosed with barium esophagogram, esophagoscope, CT and MRI. Treatment for symptomatic tumors is surgical resection. Intraluminal tumors that are not large and do not have much vascularity can be removed by endoscopy. Such as leiomyoma. Intraluminal tumors can be enucleated openly or laparoscopically.
The incidence of esophageal cancer varies according to regions and countries. These geographical differences also reveal the etiological role of environmental and dietary differences on carcinogenesis. In the last 30 years, the 5-year survival rates of esophageal cancer have increased from 3% to 15%. Since it is usually detected at a late stage, survival rates are also low. is low.
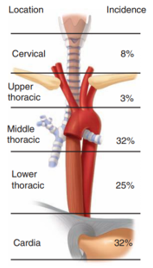
Current treatment models consist of a combination of surgery, radiotherapy and chemotherapy and lead to longer 5-year survival rates. Histologically, squamous cell cancer is the most common. While the rate is 3-5/100,000 in Western societies, it is 100/100,000 in Eastern societies.
In addition to environmental factors, low socio-economic level, race, alcohol and tobacco use,
N-nitrosamines, achalasia, caustic strictures, tylosis (foot sole and toe hyperkeratinization) and Plummer-Vinson syndrome are factors that increase the risk of squamous cell cancer. This type of cancer tends to be multicentric and is often seen in the middle 1/3 of the esophagus (55%), while cervical They are seen in 8% of the esophagus and 37% of the distal esophagus.
Fungative (60%)

ulcerative (25%) and

infiltrative (15%)

They exhibit growth type. The prognosis of invasive squamous cell cancer is poor and the 5-year survival rate after treatment is 5-12%. The annual survival rate is stated as 3% in those with positive lymph nodes and 42% in those with negative lymph nodes.
Another type of cancer is adenocarcinomas. Adenocarcinomas are often associated with Barrett's esophagus (20-58%) and involve the distal esophagus or occur when proximal gastric cancer (Cardia Ca) spreads to the esophagus. The risk of developing adenocarcinoma in patients with Barrett's esophagus is 40 times higher than in the normal population, and only the columnar mucosa showing intestinal metaplasia is thought to have malignant potential.
The initial symptoms of esophageal cancer are dysphagia (difficulty swallowing) and weight loss in 90% of cases. The slow development of dysphagia is perhaps the reason for late referral to healthcare institutions. Various degrees of odynophagia (painful swallowing) are observed in 50% of patients.
Findings such as hoarseness, abdominal pain, persistent back and bone pain, hiccup, cough and aspiration pneumonia suggest insectability. Findings detected in the physical examination are proportional to weight loss.

Enlarged cervical or supraclavicular lymph nodes, bone pain, and all neurological symptoms should be evaluated with CT or MRI.
Endoscopic evaluation is essential for histological diagnosis and intramural spread. Bronchoscopy is another necessary diagnostic tool to determine tracheobronchial involvement.
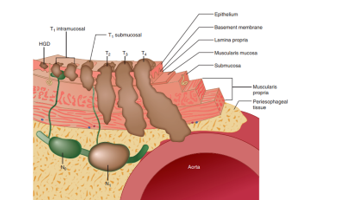
In particular, determining nodal involvement poses difficulties. CT can provide information on this issue. Endoscopic ultrasonography is superior to CT in determining esophageal wall penetration. Thoracoscopic and laparoscopic staging of esophageal cancer is recommended. It is reported that accurate staging can be achieved at a rate of 90% with this method. The most commonly used staging system today is the TNM staging system. Lymph node involvement and number, tumor penetration in the esophageal wall and distant metastases have been determined as independent factors affecting the prognosis in esophageal cancers.
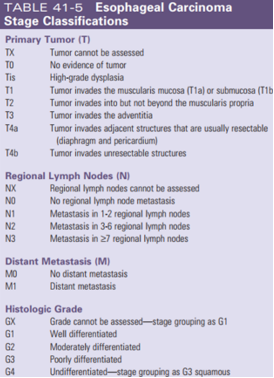
The aim of all patients with esophageal cancer is to determine the chance of surgical resection because surgical resection is the only approach that provides cure. Surgery should be performed in all patients who do not have signs of distant metastasis and who can tolerate surgery due to their physiological condition. The operative mortality of transhiatal or transthoracic esophagectomy is less than 5%, but their morbidity is 10% and 27%, respectively. While the 5-year survival rates obtained with these two approaches in Stage I and Stage II patients are 65% and 85%, respectively, this is in Stage III patients. The rate is 15% and 28%. In early stage esophageal cancers (Stage 0 and I), 5-year survival is reported as 70%. If the tumor is limited only to the mucosa, 5-year survival rates can be up to 90%. Due to the longitudinal transmural spread of esophageal cancers, the tumor's survival rate is reported to be 70%. Total or subtotal esophagectomy is required for complete removal. The incidence of local recurrence in segmental resections is extremely high. Adjuvant chemotherapy and radiation therapy have positive effects on survival.
Subtotal esophagectomy; Subtotal esophagectomy can be performed in tumors located in the gastroesophageal junction. Ivor-Lewis (Tanner-lewis) esophagectomy is a suitable surgical intervention.

Total esophagectomy; In proximally located tumors (cervical or upper esophageal region), segmental resection (Ivor-Lewis) total esophagectomy is required due to the difficulty of obtaining a negative anastomosis line. Two methods are widely used for total esophagectomy. In the first of these, the esophagus is mobilized with a right thoracotomy and anastomosed in the neck. In the second one, it is mobilization of the esophagus transhiatally and anastomosis in the neck without performing thoracotomy. Today, especially Japanese surgeons use 2 different types of radical lymphadenectomy techniques in esophageal cancer surgery.
Dual-site lymph node resection
Three-site lymph node resection
As the results of neoadjuvant treatments, which are increasingly used in recent years, are better than radical lymphadenectomy, many surgeons have avoided radical lymphadenectomy, which has higher morbidity and mortality.
Reconstruction after resection; After esophagectomy, the stomach, colon and jejunum are used for reconstruction. In cases where the stomach is not suitable, the colon is the second most commonly used option. The alternative to stomach and colon interposition is free jejunal graft.
Palliation in unresectable tumors; In recent years, there has been a dramatic increase and success rate in these methods. Patients with tracheoesophageal fistula are now treated with stents rather than bypass. Endoscopic laser treatment, electrocoagulation, photodynamic therapy are the main methods of these methods and the reported success rates are between 80-100%.
Radiotherapy is widely used alone or in combination. Studies show that radiotherapy and chemotherapy should be used in combination for palliation purposes, unless there is a contraindication to the use of chemotherapy. The most commonly used agents are; 5-fluorouracil, cisplatin, mitomycin C and methotrexate. The addition of paclitaxel gave promising results.
The 5-year survival rates achieved with curative surgery in esophageal cancers are very low, around 20% and between 10-35%. The benefits of neoadjuvant approaches are the decrease in tumor stage and the shrinkage of the tumor mass and the resulting increase in curative resection rates, and the early treatment of micrometastases. Neoadjuvant alone 5-year survival after chemoradiotherapy was around 27%, and with the addition of surgery, 5-year survival rates could be increased to around 67%. However, this treatment also caused an increase in morbidity and mortality rates.
If you want to read our article about esophageal cancer; https://www.erhuneyuboglu.com/yemek-borusu-kanseri