Gastroesophageal Reflux Disease
Content is being updated......

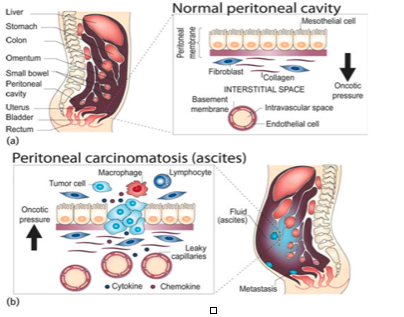
Peritoneal spread is a common form of cancer spread (metastasis). The benefits of administering chemotherapy directly into the abdominal cavity are supported by preclinical and pharmacokinetic data. Compared to intravenous treatment, intra-abdominal administration of chemotherapy results in a drug concentration and effect several times higher in the abdominal cavity.
Recent clinical trial results show that intra-abdominal chemotherapy provides some advantages in terms of survival (life expectancy) in different tumor types such as ovarian, colon and gastric tumors. However, due to the toxicity of the drugs given in intra-abdominal chemotherapy, the practice has not yet become universal. On the other hand, the distribution of the prepared chemotherapeutic fluid in the abdomen and its penetration into the tissue may be insufficient. A new way of administering intraperitoneal chemotherapy is "pressurized aerosol chemotherapy", in which cytotoxic (cancer cell-killing) drugs are administered into the abdomen with a special device.
Pressurized intraperitoneal aerosol chemotherapy can be performed laparoscopically with balloon trocars in a specially designed operating room.
First, the abdomen is inflated with carbon dioxide gas at normal temperature with a pressure of 12 mmHg, as in conventional laparoscopy. Chemotherapy solution is prepared at a dose of approximately 10% of the normal systemic dose (intravenous chemotherapy). It is administered into the abdomen as pressurized-aerosol for 30 minutes with Kapnopen passed through a trocar previously placed in the abdominal wall. At the end of the operation, the aerosol is drained with a closed suction system. Aerosol administration into the peritoneal cavity ensures homogeneous distribution of chemotherapy drugs into the abdomen.
Tumor cell fluid pressure is a major obstacle in cancer treatment. This pressure overcomes the internal fluid pressure of tumor cells and allows drugs to penetrate into the tumor. This results in higher local drug concentrations compared to conventional intravenous and intra-abdominal chemotherapy. On the other hand, the plasma concentration of chemotherapy drugs remains lower, resulting in minimal side effects and organ toxicity. Initial clinical studies are very promising for the results of pressurized aerosol chemotherapy (PIPAC) in cancer types such as peritoneal cancer, colon cancer, gastric and ovarian cancer. In addition, side effects have been observed to be very low.
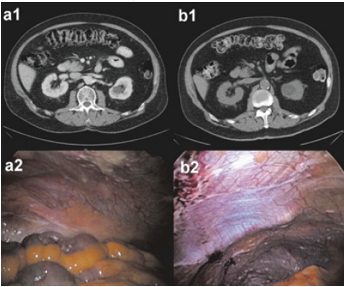
Peritoneal carcinomatosis (diffuse cancer in the abdomen) is difficult to diagnose. Imaging techniques such as computed tomography and MRI can help plan surgical intervention. However, since these examinations have low sensitivity in the diagnosis of small-volume disease, they may be insufficient in the detection of localized peritoneal carcinomatosis. Therefore, direct visualization of the peritoneum (peritoneum) by laparoscopy or laparotomy is the "Gold Standard" in the diagnosis of peritoneal carcinomatosis.
Diagnostic Studies
The investigations necessary to determine the best course of treatment for patients with peritoneal carcinomatosis can be listed as follows.
Imaging studies are essential in patients with known or suspected peritoneal cancer. Although there have been significant improvements in imaging techniques in recent years, adequate detection of peritoneal invasion is sometimes difficult due to the size, morphology and localization of the masses.
1.Computed Tomography (CT Scan): Contrast-enhanced computed tomography is the standard imaging modality for the diagnosis of peritoneal carcinomatosis (peritoneal cancer invasion), although its accuracy in detecting small peritoneal involvement remains limited. However, there is a 30-45% risk of missed lesions smaller than 5 mm.
2.MRI (Magnetic Resonance Imaging): Especially diffusion weighted images provide valuable information in the evaluation of peritoneal carcinomatosis. However, it cannot be used routinely because it is more expensive and cannot be performed everywhere.
3.Ultrasound: Ultrasonography is not a routinely used method in the follow-up of the patient who will undergo pipac. Because the detection of tumor regression or, on the contrary, progression may be subjective and dependent on the interpretation of the person performing the ultrasound. In addition, in the case of a single measurable lesion located only in the paraaortic area, a healthy evaluation may not be possible due to the obstruction of intestinal gases.
4.PET/CT: FDG-PET/CT can be of great benefit in planning the treatment of HIPEC in terms of detection of tumoral lesions larger than 1cm (PPV - positive predictive value 93-100%). However, its sensitivity is low in the presence of millimetric disease. Compared to other imaging modalities, PET/CT is the most useful method in patients with peritoneal carcinomatosis. However, it may be insufficient in small nodules and is more expensive than others.
5.Diagnostic Laparoscopy: Preoperative assessment of the extent of peritoneal carcinomatosis is difficult; a clear assessment is often made during surgical exploration. Staging with conventional imaging methods can often be limited, leading to incorrect staging or unnecessary laparotomy (opening the abdomen through incision). Diagnostic laparoscopy can provide detailed information about intra-abdominal cancer and histologic confirmation of suspected peritoneal carcinomatosis. It can also be used effectively to evaluate the effects of neoadjuvant (preoperative) chemotherapy.
6.Peritoneal Cancer Index: (PCI) There are some scoring systems for evaluating the degree or extent of peritoneal carcinomatosis. These are; Gilly staging, Japanese gastric cancer P score, Peritoneal cancer index (PCI) and Simplified peritoneal cancer index (SPCI). The most widely used of these is the "peritoneal cancer index", which is a scoring system that determines and standardizes the prevalence of peritoneal carcinomatosis. In this scoring system, the abdomen is divided into 9 regions. The umbilical region is taken as 0, starting from the right upper quadrant, each region is numbered clockwise. 9-12 are the numbers given to the small intestine sections. Lesion size (LS) is used to identify peritoneal nodules.
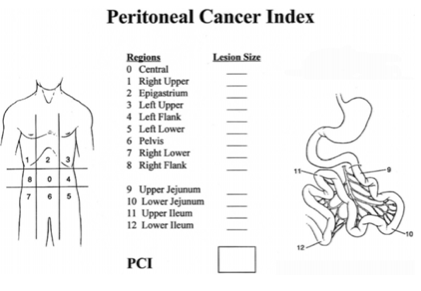
The primary tumor to be removed and recurrences at the primary site are excluded.
In pseudomyxoma peritonei (cancer of the peritoneal lining itself) or low aggressiveness mesotheliomas, the PCI is considered to be 39 (13 sites * LS 3 = 39), and the PCI can be returned to 0 because the disease is non-invasive with surgery. If the PCI score is low but there is invasive cancer localization in vital anatomical areas (such as patients with invasive carcinoma with extensive small bowel involvement and no need for general cytoreduction), then the desired cancer clearance cannot be achieved. These patients should be considered as patients with bone or lung metastases and only palliative surgery should be performed.
7.Peritoneal or Pleural Cytology: Peritoneal lavage cytology (the search for cancer cells from fluid taken from the abdomen) can be performed as a complementary staging parameter in patients at risk of peritoneal carcinomatosis.
Gastric Cancer: The 13th revision of the Japanese classification of gastric cancer recommends cytologic examination of ascites or peritoneal fluid during surgery.
Ovarian Cancer: The current German S3-guideline recommends peritoneal lavage and cytology during surgical resection as a routine part of staging.
Colorectal Cancer: The current German S3-guideline does not make any recommendations regarding cytology in colorectal cancer.
Until recent years, both peritoneal and pleural carcinomatosis were known as conditions without treatment options in terms of quality of life and prolongation of life expectancy. Even if the disease cannot be completely eliminated, some current forms of treatment have emerged that can be applied systemically and locoregionally.
These treatment options for patients with peritoneal carcinomatosis can be listed as follows:
Intraperitoneal chemotherapy strategies are presented in the table below.
Abbreviation Definition
CHPP Continuous hyperthermic peritoneal perfusion
NIPS Neoadjuvant intraperitoneal-systemic chemotherapy
HIPEC Hyperthermic intraperitoneal chemoperfusion
EIPL Extensive intraoperative peritoneal lavage
EPIC Early postoperative intraperitoneal chemotherapy
Because of these complex options in the treatment of peritoneal carcinomatosis, it is beneficial to perform interventions in a mutidisciplinary manner.
Aerosol delivery of drugs into the abdominal cavity (into the peritoneal cavity) using the physical properties and pressure of the gas (therapeutic capnoperitoneum) is a form of treatment proposed in 1999. The treatments applied in this way are considered as a revolution in laparoscopic surgery. The advantages of aerosolizing certain special drugs are well known, especially in the treatment of lung diseases.
In this way, the drugs show their effect more quickly, lower doses are used compared to intravenous or oral doses, and the frequency of systemic side effects is lower. In addition, the use of aerosols avoids toxic effects of the drug on the liver and digestive system. The combination of aerosol delivery with artificial hydrostatic pressure provides further synergy.
It can be defined as a suspension of particles (liquid droplets in Pipac) in a gas (here carbon dioxide). There are hundreds of aerosol products on the market, including medical ones. Usually an inert gas acts as a propellant under pressure. The function of this propellant component is to create a solvent effect on the product, dragging the product and pushing it out of the container.
PIPAC technology works a little differently than aerosol technology, there is no need for a propellant gas.During PIPAC, the liquid drug solution is aerosolized into a carbon dioxide gas-filled container by means of a special device (Kapnopen-Micropump -MIP).During PIPAC, the micropump does not form a monodisperse aerosol (all particles are of the same size), on the contrary, it forms a polydisperse aerosol (particles of different sizes).
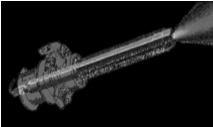
Micropump
Current pipac technology allows aerosolization of high density solutions such as polymers, glucose and lipids. It has also been shown to work under conditions of high moisture saturation. In other words, it can create fog within fog. Aerosols used in the medical field create a fog-like state, with particles smaller than 50 microns in size, so that the dispersed particles or particles remain suspended in the fog for long periods of time. A typical 1-second space spray generates 120 million particles, a significant proportion of which remain suspended for 1 hour. The size of the microdroplets produced during PIPAC is approximately 11 microns, and it is easy to see that microdroplets are still floating in the abdominal cavity after 30 minutes of PIPAC.

Micropompa (particles are seen flying during surgery)
In experimental animal studies, it has been shown that increasing intra-abdominal pressure increases the antitumoral effects and antitumoral accumulation of doxorubicin and cisplatin (cancer cell killing drugs) administered into the abdomen. Increased intra-abdominal pressure creates convective flow, allowing the drug to pass from the peritoneal cavity to the subperitoneal space. At the same time, intra-abdominal pressure creates a counter-gravity on hydraulic capillary pressure, slowing the excretion of the drug from body parts.
It is an instrument for effective aerosolization under normal laparoscopic conditions.(MIP) MIP (micropump) has a diameter of 9 mm. It consists of three parts: connection inlet, body part and spray tip. MIP should only be used by a physician who has received training in this area.MIP should only be used in a closed abdominal or thoracic cavity.MIP is inserted into the abdominal cavity under videoendoscopic visualization using a 10-12 mm balloon trocar.The abdomen should be thoroughly examined before the procedure begins. In case of doubt, the entire abdomen should be covered with a protective adhesive film. Only non-leaking trocars should be used and the safety valves of the trocars should be closed.
MIP should only be performed in the operating room with laminar flow and all air should be exchanged every four minutes maximum. MIP must be done with a device that can be controlled remotely from outside the operating room. The ventilation system of all operating rooms must be DIN 1946 Part 2 " It must comply with the norms "Ventilation - Health technical requirements" and DIN 4799 "Testing of air control systems in operating rooms".
The high-pressure injector is connected to the micropump via a high-pressure connection line, and the prepared therapeutic drug (chemotherapy drugs) is delivered to the micropump with a pressure of 20 bar. During the use of high-pressure injectors, there are potential hazards for the patient, surgical team or other persons (air embolism, contamination, etc.).
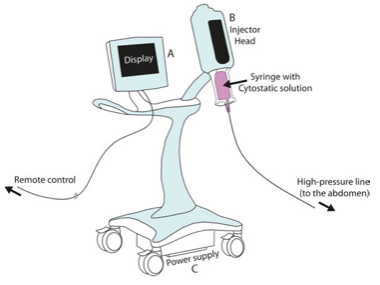
After the abdomen is inflated with carbon dioxide at 37 0 C, two balloon trocars (Applied Medical) are inserted into the abdominal wall. The abdomen is laparoscopically explored (fully visualized and examined) and the peritoneal cancer index (PCI) is determined. The ascites is drained and biopsies are taken from the abdominal wall. The nebulizer (MIPR, Reger Medizintechnik) is connected to a high-pressure injector (Injectron 82M, MedTron) and inserted through the trocar into the abdomen.
Cisplatin 7.5mg/m2 in 150 ml 0.9% NaCl followed by Doxorubicin 1.5mg/m2 in 50 ml 0.9% NaCl as pressurized aerosol. The system is then kept closed for 30 minutes (application time), after which the toxic aerosol is discharged through the closed system and the trocars are removed. PIPAC is a procedure that can be repeated 2 to 5 times at different time intervals.